

Meniscus Tear
The knee joint is formed where the femur (the thigh bone) meets the tibia (the long shin bone of the lower
leg). Sitting in front of the joint is a third, smaller bone--the patella. This bone is commonly referred to as the
"knee cap." The lower end of the femur forms two round portions known as condyles. The shallow groove
between the condyles on the front of the femur provides a place for the patella to glide up and down as the
knee bends and extends. This is called the trochlea. The top of the tibia is known as the tibial plateau. It is
relatively flat in comparison to the femoral condyles.
The surfaces of the femoral condyles, tibial plateau, and the back of the patella are capped with a layer of
cartilage. The cartilage that caps the ends of bones in joints is known as articular cartilage. Articular
cartilage is smooth and slippery. This lowers friction in the joint and allows the bones to glide smoothly against
one another as the knee moves. Articular cartilage is slightly softer and more rubbery than bone. A thick,
viscous fluid known as synovial fluid (joint fluid) fills the joint. Together, the articular cartilage and synovial
fluid provide a cushion between the bones. The joint is surrounded by a capsule known as the synovium which
keeps the synovial fluid from leaking out.
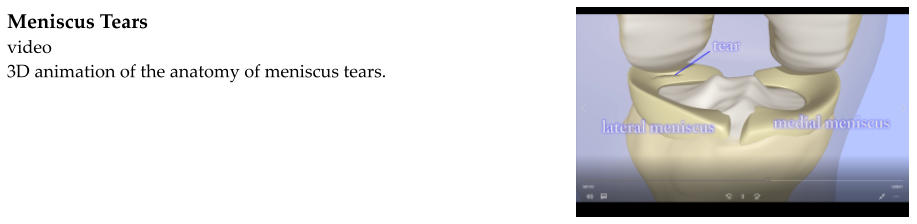
A wedge-shaped meniscus sits on each side of the knee. The meniscus is made of rubbery cartilage. It helps to
fit the round condyles of the femur to the flat tibial plateau. This helps to maintain knee stability. The
meniscus is commonly described as the "shock absorber" of the knee. Along with the articular cartilage and
synovial fluid, it helps to minimize the impact between the femur and tibia when the knee is bearing weight.
The meniscus on each side of the knee curves around the edge of the tibial plateau, forming a "C". The
meniscus on the outside of the knee is called the lateral meniscus. The meniscus on the inside of the knee is
called the medial meniscus.
Each meniscus curves along the edge of the tibial plateau. The curve along the front of the tibia is called the
anterior horn. The curve along the back of the tibia is called the posterior horn.
Like most cartilage structures, the meniscus does not have a very good blood supply. The outer edge where it
attaches to the joint capsule has the best blood supply. This is known as the "red zone." The inner edge has
virtually no blood supply. This is known as the "white zone." The space in between is called the "red-white
zone." It has better blood supply than the white zone, but worse blood supply than the red zone.
Injury to the Meniscus
A meniscus tear may occur because of a traumatic injury to the knee. This is known as an acute tear. Acute
tears usually occur with a violent pivoting and twisting motion. They are more common in young athletes.
Acute meniscus tears frequently occur with other knee injuries including ACL tears.
As the knee ages, the cartilage begins to succumb to wear and tear. Just as the articular cartilage wears away
in osteoarthritis, the meniscus can begin to degenerate as well. As it becomes weaker and less healthy, it
becomes easier to tear. Simply taking a bad step can tear the meniscus. This is known as a degenerative tear.
The blood supply to the meniscus is poor. Without a healthy blood supply, nutrients are not readily available to
the cartilage tissue. When it is damaged, it does not heal as well as bone, skin, muscle, or other tissues.
The meniscus can tear in a variety of ways. The appearance and orientation of the tear can be described as
longitudinal, bucket handle, parrot beak, flap, radial, etc. The location is described as the anterior horn,
posterior horn, or middle third. It is also important to identify whether the tear is located in the red zone, red-
white zone, or white zone.
Meniscus tears have a tendency to flip over and catch in the joint. This causes mechanical symptoms such as
clicking, catching, and locking up of the knee. Bearing weight on the torn meniscus typically causes pain. The
torn portion of the meniscus may also rub against the articular cartilage in the knee, wearing at the cartilage
and perhaps speeding up the degenerative process.
Diagnosing a Meniscus Tear
History
People with meniscus tears complain of pain within the knee joint. They may complain of pain with bearing
weight. They may also complain of mechanical symptoms such as clicking, catching, and locking up. The knee
frequently "gives out."
Knee pain usually begins with an injury. In younger patients this is usually a more traumatic injury such as
twisting the knee while participating in a sport. In older patients, the injury may be surprisingly mild such as
stepping onto uneven ground
Some people with degenerative tears may not remember any injury. They report a gradual onset of knee pain.
ྕ
Knee pain
ྕ
Mechanical symptoms: clicking, catching, locking up
ྕ
Giving out
ྕ
Injury in younger people, maybe not in older people
Physical Exam
A thorough physical examination seeks not only to find evidence of a meniscus tear, but also to rule out other
causes of knee pain such as fractures, bursitis, osteoarthritis, nerve damage, etc. Meniscus tears are not
associated with any visible deformity of the knee, although there may be mild swelling. Knee pain and
mechanical symptoms may cause the person to limp. The knee is usually very tender along the joint line (the
space between the femur and tibia on the side of the knee) where the meniscus is torn. If the meniscus tear is
flipped over and catching, it may limit range of motion of the knee. Some people seek care when they are
unable to fully extend or flex the knee.
Special knee maneuvers have been designed to test for meniscus tears. They include McMurray's test and
Apley's test.
During McMurray's test, the knee is flexed and the examiner's hand is held on the knee with the thumb or
finger on the joint line over the meniscus. To test for a medial meniscus tear, the knee is bent slightly outward
(valgus stress) and rotated outward (external rotation) and slowly extended. To test for a lateral meniscus
tear, the knee is bent slightly inward (varus stress) and rotated inward (internal rotation) and slowly extended.
If this causes pain and a click at the joint line, it is most likely a meniscus tear. If it causes pain but no click or
clunk is felt by the examiner it may be a meniscus tear but could also be another problem such as arthritis.
During Apley's test, the person with knee pain lays on their belly. Their knees are bent so their feet are up in
the air. Downward pressure is applied to the leg, pushing the tibia into the femur. The knee is gently rotated
in and out. If this causes pain, a meniscus tear is suspected.
Inspection: normal or mild swelling
Passive range-of-motion (the person with knee pain relaxes while the examiner bends and straightens
the knee for them) and active range-of-motion (the person with knee pain attempts to bend and
straighten their own knee) may be limited, especially if the meniscus tear is displaced and catching in
the joint. Normal range-of-motion:
o
Flexion ≈ 130°
o
Extension ≈ 0°(completely straight leg)
Tenderness along the joint line over the meniscus
McMurray's test: Pain and click indicates meniscus tear. Pain suggests possible meniscus tear.
Apley's test: Pain suggests possible meniscus tear.
X-rays
While a torn meniscus cannot be visualized on x-rays, x-rays are very helpful with uncovering other sources of
knee pain such as fractures, chondrocalcinosis (calcification of the meniscus), loose bodies (pieces cartilage
floating in the knee joint), and arthritis.
Depending on the severity of the degenerative changes, osteoarthritis can often be readily identified on x-rays.
X-rays will demonstrate narrowing of the joint space between the femur and tibia. They may also demonstrate
osteophytes (bone spurs) and sclerotic bone (bone that appears more white on x-rays because it has hardened).
MRI (magnetic resonance imaging)
An MRI is the imaging test of choice for identifying meniscus tears. The meniscus can be visualized on an MRI as
a black triangle. A tear appears as a white line or splotch through the meniscus. The MRI can be used to
determine the location of the tear and may provide information as to whether the tear is repairable or not.
Other knee problems can also be discovered on an MRI including arthritis, ligament sprains and tears (including
ACL tears), chondral injuries (injuries to the articular cartilage), etc.
Knee Arthroscopy
While MRIs are very helpful and identify the vast majority of meniscus tears, occasionally someone with have a
normal appearing MRI with continued knee pain. If conservative treatment including NSAIDs, ice, elevation,
rest, physical therapy, and perhaps a steroid injection are not effective, diagnostic knee arthroscopy (knee
scope) may be performed to search for a source of knee pain.
Knee arthroscopy involves introducing a slender camera called an arthroscope into the knee joint. The inside
of the knee joint can then be viewed on a monitor. During the knee scope procedure, the menisci are
examined. A small, metal probe can be used to examine each meniscus.
Treating Meniscus Tears
The goal in treating degenerative meniscus tears without mechanical symptoms is to alleviate pain. Older
people with arthritis and degenerative meniscus tears may find relief with NSAIDs, steroid injections, ice,
elevation, and rest. While the tear will not heal, pain will likely improve without surgery. If symptoms do not
improve over time, knee arthroscopy may be recommended.
Acute meniscus tears, tears in younger people (under about 50 years old), and tears that cause catching and
locking are almost always treated surgically.
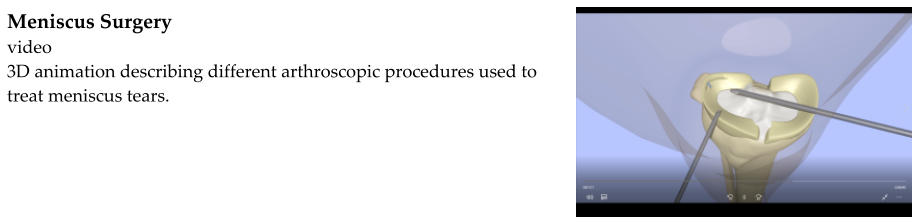
Surgery for a torn meniscus is most commonly done arthroscopically (knee scope) and under general anesthesia
(asleep). It is an outpatient procedure, meaning that the person can go home after surgery. Small incisions are
made, just large enough to pass a slender camera and instruments into the joint. These small incisions are
known as the arthroscopic portals. Sterile water is allowed to flow into the knee joint to allow the surgeon to
see and to keep bleeding to a minimum. The surgical team is able to see the inside of the knee joint on a
monitor connected to the camera. The torn meniscus is visualized and the rest of the knee joint is examined to
look for other possible sources of knee pain.
Once the surgeon has examined the torn meniscus, the decision must be made to excise the torn portion or
repair it. Meniscal repair is not a good option in people with degenerative tears or arthritis. However, in
young athletes it is important to preserve the meniscus if possible. Tears located in the red zone (the outer
edge of the meniscus where it attaches to the joint capsule) can often be repaired.
Partial Meniscectomy
If a meniscus tear is not repairable, a partial meniscectomy is performed. This means that the torn portion of
the meniscus is removed, leaving as much of the healthy meniscus intact as possible.
Recovery after a partial meniscectomy is quick. Full weight-bearing is permitted after the procedure. The
pain caused by the meniscus tear is immediately relieved, but it may be replaced by some mild postoperative
pain.
Meniscal Repair
Repairing a torn meniscus involves pushing the torn flap back into place and stitching it back together. Several
methods have been developed.
Open repair: An incision is made over the meniscus rather than attempting to do the repair
arthroscopically. The meniscus is exposed and the torn portion is repaired with suture.
Inside out: The torn meniscus is visualized using the scope. An additional incision is made on the side
of the knee over the meniscus to expose the joint capsule. Suturing instruments are passed into the
knee joint using the arthroscopic portals. Suture is passed from the inside of the knee joint, through
the torn meniscus, and out the joint capsule. The suture knot is then tied. A sufficient number of
sutures are placed to repair the tear. The instruments are removed and the larger incision over the
joint capsule is closed.
Outside in: The torn meniscus is visualized using the scope. An additional incision is made on the side
of the knee over the meniscus to expose the joint capsule. Suture is passed from the outside of the
capsule, through the torn meniscus, and into the knee joint. The suture knot is then tied within the
joint. A sufficient number of sutures are placed to repair the tear. The instruments are removed and
the larger incision over the joint capsule is closed.
All inside: The torn meniscus is visualized using the scope. Special instruments are passed through
the arthroscopic portals into the knee joint. Several orthopedic equipment companies have developed
instruments capable of passing suture through the meniscus and anchoring it to the joint capsule
without making a separate incision over the joint capsule. The suture knots are tied within the joint
using the special instruments. A sufficient number of sutures are placed to repair the tear and then
the instruments are removed.
After surgery the repaired meniscus must be protected while it heals. The person is not permitted to bear
weight for several weeks following the procedure. Gentle range of motion exercises within limits designated by
the surgeon are recommended to keep the knee from getting too stiff. Once the meniscus has had sufficient
time to heal, weight-bearing will be permitted. Physical therapy is often recommended to help regain strength
and range of motion.
Meniscal Transplant
A large tear of the meniscus that cannot be repaired may result in the removal of most of the meniscus. This
can result in chronic pain and a sensation of instability. In very select people, a meniscal transplant may be an
option.
A meniscus is harvested from a cadaver and implanted in the knee to take the place of the damaged meniscus.
Meniscal transplants are not as common as partial meniscectomy and meniscal repair. They are not successful
in people who have too much arthritis or other knee problems.
In summary, surgical options for meniscus tears include:
Arthroscopic partial meniscectomy
o
Irreparable meniscus tears
o
Older people and people with degenerative changes
o
Weight-bearing permitted following surgery
o
Quicker recovery
Arthroscopic meniscal repair
o
Tears in the red zone (outside edge)
o
Younger, more active people
o
No weight-bearing for several weeks after surgery
o
Longer recovery
o
Seeks to preserve the meniscus to prevent developing other knee problems in the future
Meniscal transplant
o
Large, irreparable tears resulting in removal of most of the meniscus
o
Less common, newer procedure
o
Only an option in very select people
o
Recovery Following a Knee Scope with Partial Meniscectomy
Walking and full weight-bearing is permitted after surgery if the only procedure performed was a partial
meniscectomy. Range of motion exercises are permitted, but activity should be limited for the first couple of
days to prevent pain and swelling. The knee should be iced as much as possible, taking care to keep the ice
from sitting directly on the skin as this may burn the skin. The knee should also be elevated. Ice and elevation
are important to prevent postoperative swelling.
Stitches may or may not be present over the portal incisions. If so, they are removed about 1 week after
surgery.
Recovery Following a Knee Scope with Meniscal Repair
A meniscal repair is meant to hold the torn flap of meniscus in place. It is not meant to withstand the forces
that come with walking and full weight-bearing. Weight-bearing is not permitted for several weeks after
surgery. The knee may be protected in a brace. Crutches are provided to avoid placing any weight on the
knee.
The knee should be iced as much as possible, taking care to keep the ice from sitting directly on the skin as this
may burn the skin. The knee should also be elevated. Ice and elevation are important to prevent
postoperative swelling.
Stitches may or may not be present over the portal incisions. If so, they are removed about 1 week after
surgery.
Range of motion exercises are begun within limits set by the surgeon. Over time, range of motion limits are
increased and weight-bearing can begin.
Muscles involved in walking and moving the knee begin to atrophy because they are not being used normally
while non-weightbearing. Physical therapy is helpful for maintaining range of motion and strengthening the
knee.
Expectations Following Meniscus Surgery
Immediately following surgery, meniscus pain will be replaced with postoperative pain. This is usually mild.
Pain will improve over the first couple of days.
Most people who undergo a partial meniscectomy, including athletes, are ready to return to their normal
activity level within 2 weeks. The success rate is high.
Most people who undergo a meniscal repair are ready to return to their normal activity level within about 3
months. The success rate is high, but repairs do fail. If so, pain will persist. Some people have to return for
another knee scope. The second time, a partial meniscectomy may be performed.



















