

Degenerative Joint Disease of the Knee
Knee osteoarthritis is damage to the cartilage in the knee joint that occurs over time.
Articular cartilage is a smooth lining that caps the ends of bones where they come together in joints. This protects
the ends of the bones and allows them to glide painlessly against each other with movement and bearing weight.
Osteoarthritis is a condition in which the cartilage begins to wear away. Without the padding and smooth surface
that the cartilage provides, the bones begin to grind against each other. This results in pain, especially with bearing
weight on the joint, and stiffness. Osteoarthritis is also known as degenerative joint disease or simply arthritis.
"Chondromalacia" is a term that means "softening of the cartilage." It is often used to describe the wear and tear of
cartilage in osteoarthritis.
Factors that contribute to developing osteoarthritis include age, injuries, lifestyle, weight, and genetics.
It has been said that everyone who lives long enough gets arthritis. Articular cartilage does not have as much
potential to heal as bone, skin, and other tissue. Injuries to the knee can crack the cartilage. Once a crack has
started, it is easier for the cartilage to begin to peel away. More stress on the knee causes more wear and tear. And
so obesity, jobs that require a lot of standing and walking, and other lifestyle factors can speed up the degeneration
of the joint. Arthritis at an earlier age seems to run in families, and so there is thought to be a genetic component as
well.
Symptoms of knee osteoarthritis include pain (especially with bearing weight), swelling, and stiffness.
Arthritic knee pain is worse with movement and bearing weight. Many people complain of pain with attempting to
get up out of a chair and with climbing steps. Pain usually begins gradually and slowly worsens. However, some
people do not realize they have arthritis until after an injury. Because they don't have as much protection from the
cartilage, the injury is more painful and takes longer to resolve. The knee sometimes swells and at times quite a bit
of fluid can collect. This is known as an "effusion," or "water on the knee." Grating and grinding is another common
complaint. Severe arthritis can result in deformities. If one side of the knee wears down more quickly than the
other, a varus (bow-legged) or valgus (knock-kneed) deformity can occur.
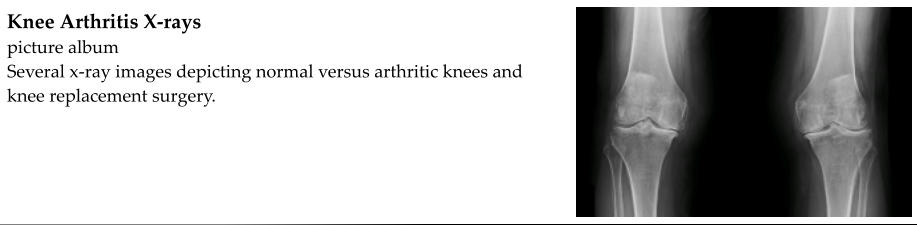
Knee osteoarthritis is diagnosed based on symptoms, a physical exam, and x-rays.
The diagnosis of degenerative joint disease, or osteoarthritis, is often made clinically based on the person's age, the
location and type of pain, a gradual onset of pain, and improvement with conservative treatment such as NSAIDs
and steroid injections. In more advanced osteoarthritis, degenerative changes are easily recognized on x-rays. The
joint space narrows, sometimes with bone-on-bone apposition. Bone spurs (osteophytes) may form. In early
arthritis, degenerative changes might not be visible on x-rays but may be seen on an MRI.
Treatment for knee osteoarthritis includes NSAIDs (such as ibuprofen), steroid injections, hyaluronate injections,
physical therapy, bracing, topical creams and ointments, lifestyle modifications, knee arthroscopy (knee scope), and
knee replacement surgery.
Arthritis medications are known as NSAIDs (non-steroidal anti-inflammatory drugs). They help reduce the
inflammation associated with osteoarthritis which helps with pain and swelling. Examples of NSAIDs include
ibuprofen, naproxen, diclofenac, meloxicam, and celecoxib. While NSAIDs are relatively safe when taken as directed
or prescribed, they are not without risks and side effects. NSAIDs can result in stomach problems such as ulcers and
bleeding, especially if they are taken in high doses or for long periods of time. They can also be hard on the kidneys
and should not be taken by people with poor kidney function. People with high blood pressure may have more
difficulty controlling their blood pressure if they are taking NSAIDs. People who take blood thinners should avoid
NSAIDs.
Steroid (cortisone) injections are frequently given in the knee to reduce pain and swelling. How long the steroid
injection relieves pain varies widely from person to person. Some people, especially those with more severe arthritis,
may not get much relief. Others return every several months for an injection because it has been very effective.
Steroid injections are relatively safe. However, they are not without risks. There is a very small risk of introducing
bacteria into the knee joint and causing an infection. If injections are given too frequently, it can damage the
cartilage in the joint. Some people experience a "steroid flare" and joint pain worsens temporarily. People with
diabetes may experience an increase in their blood sugar for several hours after the injection.
Hyaluronate injections are sometimes referred to as "rooster comb" injections. A clear gel is injected into the knee
that acts to lubricate the joint. It is also meant to improve the health of the remaining cartilage. Hyaluronate
injections are expensive and some insurance companies refuse to cover them. Risks include infection and an allergic
reaction to the hyaluronate.
Physical therapy involves stretching and strengthening exercises. This may improve the strength and stability of the
knee. Improved mechanics in the knee pay take pressure off of more arthritic areas and help with pain and function.
Sometimes, however, the extra motion and strain of physical therapy only makes arthritic knee pain worse.
Some people with knee arthritis wear wraps, sleeves, and braces. They feel that this relieves some of their pain and
gives them a sensation of stability. "Unloader" braces are made specifically for knee arthritis. The idea is to
"unload" the more arthritic side of the knee by applying force to the sides of the knee.
Many creams, salves, and ointments have been created with the purpose of relieving joint pain. Menthol and
camphor are used in several of these products to provide a warm and cold sensation that seems to provide limited
pain relief. Other pain creams, including creams that contain anti-inflammatories and narcotics, are only available
with a prescription. Over-the-counter creams are relatively inexpensive, but "compounding" prescription creams
can be very expensive and are often not covered by health insurance.
Lifestyle changes such as weight loss, low-impact exercise, and avoiding certain activities can play an important role
in the treatment of osteoarthritis. Less weight that a joint has to sustain means less pain and slower degeneration.
High impact exercise such as jogging can be hard on the articular cartilage and, in people with arthritis, can be too
painful. Low impact exercise such as swimming and water aerobics provides good exercise that strengthens muscles
and bones without wearing away at the knee joint. Some people have to change employment because their duties at
work are too demanding on their knees.
Knee arthroscopy is a surgery in which a small camera is introduced into the knee joint to examine the cartilage.
Damaged cartilage can be debrided and smoothed, loose pieces of cartilage can be removed, and bone spurs can be
shaved down. However, in osteoarthritis the damage to the articular cartilage is too widespread to be repaired.
Degeneration will continue. While knee arthroscopy may temporarily relieve some or all of the pain caused by
arthritis, it is not a definitive treatment and pain will eventually return.
Knee replacement surgery is the definitive treatment for severe osteoarthritis.
Total knee arthroplasty, or knee replacement surgery, is a very common procedure used to treat knee arthritis. An
incision is made lengthwise on the front of the knee. The bones in the knee joint are exposed. The arthritic ends of
the bones are removed and replaced with metal implants. A plastic spacer is placed between the metal implants.
The wound is then closed. Knee replacement surgery is usually done under general anesthesia, but a regional block
is often given as well to numb the leg. A short stay in the hospital is typically recommended. Full weight-bearing is
encouraged the day of or the day after surgery. Many people are still using a cane or walker at two weeks, but most
people are walking without assistance and pleased with the result by six weeks.
Knee replacement surgery is the most definitive but also the most invasive treatment for osteoarthritis. Infection,
loosening or breakage of the implants, poor alignment, and other complications can result in chronic knee pain or
worse following surgery. Infection, although rare, can be catastrophic. People with active infections, wounds, and
poor wound healing should not undergo knee replacement surgery. Surgery can also be demanding on the heart and
other organs. People with significant heart disease or other medical problems may not be good candidates for knee
replacement surgery.
Knee replacements are expected to last about 15 years, but this varies from person to person. The knee replacement
will eventually begin to wear out or loosen. This may require a revision knee replacement. In other words, the old
implants are removed, the bone is re-cut, and a new prosthesis is implanted. Outcomes following a revision knee
replacement are generally not as good as outcomes following the first knee replacement. This is why knee
replacement surgery is discouraged in younger people. The ideal candidate is about 65 years of age.







