

Ankle Fracture
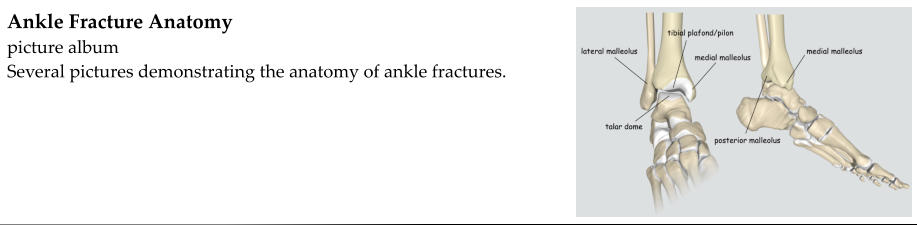
The ankle joint is formed where the fibula, tibia, and talus come together. The lateral malleolus of the
fibula and the medial malleolus of the tibia form a mortise in which the talus sits.
The term “ankle fracture” typically refers to a fracture of the lateral malleolus, the medial malleolus, or
both. A broken ankle (fractured ankle = broken ankle) usually occurs as the result of twisting or
“rolling” the ankle.
“Ankle fracture” could also refer to a fracture of the talus, fracture of the calcaneus, or fracture of the
tibial plafond.
X-rays:
•
AP, lateral, oblique (mortise view) of ankle
CT scan:
If there is need for more detailed, 3-dimensional evaluation of the fracture, a CT scan may be
obtained.
•
Need to evaluate the amount of intra-articular displacement
•
Pre-operative planning in the case of a complex, comminuted fracture
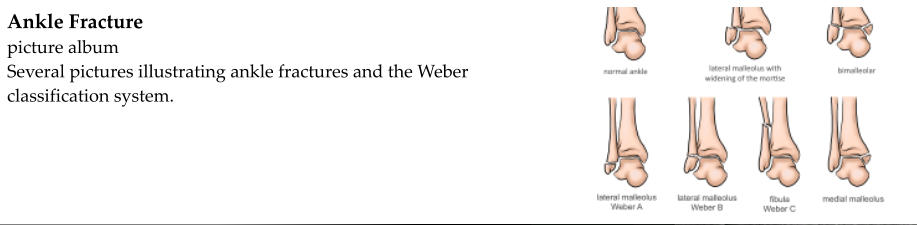
Classification:
•
Open or closed
•
Displaced or nondisplaced
•
Location
o
Lateral malleolus
o
Medial malleolus
o
Bi-malleolar (medial and lateral malleoli are both fractured)
o
Tri-malleolar (medial, lateral, and posterior malleoli are fractured)
•
Weber (based on location of lateral malleolus fracture)
o
A: fracture occurs below the level of the talar dome
o
B: fracture at level of talar dome (involving syndesmosis)
▪
B1 - just the lateral malleolus
▪
B2 - bimalleolar
▪
B3 - trimalleolar
o
C: fracture above the syndesmosis
•
Lauge-Hansen (based on mechanism of injury)
o
Supination-adduction
o
Supination-external rotation
o
Pronation-external rotation
o
Pronation-abduction
Initial management:
•
Emergent orthopedic surgery evaluation:
o
Open fractures
o
Fracture-dislocations (need reduction)
o
Compartment syndrome
•
Urgent orthopedic surgery evaluation:
o
Unstable fracture patterns
▪
Unacceptable displacement/angulation of lateral malleolus
▪
Bi/tri-malleolar
▪
Widening of ankle mortise
•
Immobilization
o
Stable fracture pattern
▪
Short-leg posterior splint
▪
CAM walker boot
o
Unstable fracture pattern
▪
Posterior splint with U-slab
▪
Bulky compression splint (Robert-Jones)
•
Pack in ice
•
Elevate
•
Non-weightbearing
•
Pain control
Definitive treatment:
•
Lateral malleolus
o
Nondisplaced or minimally displaced
▪
Acceptable alignment
•
Mortise maintained - no widening
•
No other bones involved
•
Length and alignment maintained
▪
Short-leg cast
•
May require splint to allow for swelling for 1 week following fracture
•
4-6 weeks
▪
Non-weightbearing except for exceptionally stable fractures (small avulsion fractures)
▪
Follow-up x-rays to ensure good alignment and healing
▪
Transition to walking cast or boot at 4-6 weeks as x-rays demonstrate healing
▪
After weight-bearing begins, physical therapy or home exercise program
•
Range-of-motion
•
Strengthening
•
Proprioception
o
Displaced or unstable
▪
Unacceptable alignment
•
Widening of the mortise
•
Shortening
•
Angulation
•
Bi/tri-malleolar
▪
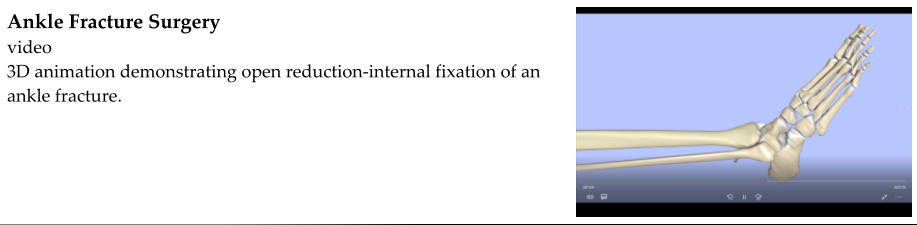
Surgical fixation
•
Open reduction-internal fixation
•
4-6 weeks non-weightbearing after surgery in cast, splint, or boot
•
Hardware does not typically need to be removed
•
Physical therapy or home exercise program
o
Range of motion
o
Strengthening
o
Proprioception
•
Medial malleolus
o
Nondisplaced or minimally displaced - casting
o
Displaced - percutaneous screw fixation or open reduction-internal fixation
•
Bi/tri-malleolar - open reduction-internal fixation
•
Lateral malleolus is the distal most portion of the fibula
•
Indications for surgical fixation
o
Displacement/angulation/shortening (< 3 mm displacement)
o
Associated fracture of the medial malleolus (bimalleolar fracture)
o
Injury to medial ligaments or syndesmosis that results in widening or instability of the ankle
mortise
▪
X-rays may demonstrate widening of the ankle mortise
▪
Stress views may be obtained to evaluate for excessive motion of the talus within the
mortise
•
Treatment
o
Nondisplaced or minimally displaced
▪
If too swollen for cast, 1 week compression splint to allow for swelling
▪
Short leg cast 4-6 weeks - neutral position
▪
Physical therapy for range-of-motion, proprioception, strengthening
o
Displaced or unstable
▪
Reduce fracture - dislocations immediately
▪
Open reduction - internal fixation as soon as permitted by swelling
•
A bimalleolar ankle fracture is when both the lateral malleolus (fibula) and medial malleolus (tibia)
are broken
•
Bimalleolar fractures are unstable
•
Treatment
o
Reduce fracture - dislocations immediately - use a compression splint to maintain good
alignment
o
Open reduction - internal fixation as soon as permitted by swelling







